May
How Researchers Are Helping Home Health Agencies with HHCAHPS Surveys
jerry9789 0 comments Burning Questions
What Are Home Health Services?
The American adult population aged 65 and older is projected to increase from 58 million in 2022 to 82 million by 2050, translating to an unprecedented 47% growth. From a 17% share of the total US population, this age group’s portion is estimated to grow to 23%.
And an aging population means more elderly adults looking to remain independent at home, in spite of the risks of various chronic conditions as well as unexpected mishaps like losing one’s balance and stumbling or falling. This is where home health services come in. Fast becoming a staple of the healthcare system, Medicare and Medicaid-certified home health agencies aim to provide “acute, chronic, and rehabilitative care from skilled and knowledgeable interdisciplinary clinical teams” while supporting elderly adults’ preferences to remain at home.
Home health services are forecasted to grow from a $100 billion to a $200 billion industry by 2028. The Centers for Medicare & Medicaid Services (CMS) pay for the majority of home health services costs, as Medicaid and Medicare make up over 60% of the US home healthcare expenses. To better evaluate, understand and improve the patient experience with home health services, the CMS has administered a survey collecting feedback from patients or their families about their skilled home care experience.
Copyright: Andrea Piacquadio
What Is A Home Health Care CAHPS Survey?
The Consumer Assessment of Healthcare Providers and Systems (CAHPS) is a program developed by the Agency for Healthcare Research and Quality (AHRQ), as requested by the CMS, which uses standardized surveys for gathering and analyzing information about patients’ experiences with healthcare services, including home health agencies. Unlike customer satisfaction surveys, CAHPS surveys focus on the patient’s experience and/or perception rather than their satisfaction with the care they’ve received. The program’s goals include the improvement of the scientific understanding of patient experience and the provision of tools for organizations to improve quality of care. The CMS publicly reports its patient experience survey results, with some surveys affecting payments to providers.
The Home Health Care CAHPS Survey (HHCAHPS), specifically, was designed to measure the experiences of people getting home health care from Medicare and Medicaid-certified home health care agencies. The first national, standardized, and publicly reported survey of home health care patients’ perspectives on their skilled home care, the HHCAHPS survey asks patients and/or their families about their experiences regarding communication between them and their providers, specific care issues, rating of care provided by the agency, and their willingness to recommend the agency to friends and family. An HHCAHPS survey is conducted by approved survey vendors through three modes: mail only, telephone only, or a mix of mail survey with a telephone follow-up for non-respondents.
The HHCAHPS survey was implemented nationally in October 2009 with home health agencies participating on a voluntary basis before quality reporting requirements for the home health annual payment update (APU) started in the third quarter of 2010. At present, the CMS requires all home health agencies receiving Medicare or Medicaid payments for serving 60 or more survey-eligible patients annually to contract with an approved HHCAHPS Survey vendor to administer the survey on a monthly basis. (Agencies serving 59 or fewer patients may apply for an exemption from the survey requirement.) The survey data is then submitted to the HHCAHPS Data Center on a quarterly basis with public reporting of survey results reflected at Home Health Compare.
Copyright: Kampus Production
What Benefits do the HHCAHPS Surveys Provide?
The HHCAHPS surveys have three broad goals:
-
-
- Produce comparable data based on patients’ experiences for objective comparisons between home health agencies
- Improve the public accountability of home health agencies with the care and service they provide
- Incentivize home health agencies to continually improve their quality of care.
-
It’s easy to think that HHCAHPS surveys influence the public reputation of a home health agency as well as the payment they could collect from the CMS. However, that view reduces the survey to the realm of “customer satisfaction,” with its attendant reliance on things like 1-to-5 scales. But instead of a pure “customer satisfaction” framework, the information gathered from HHCAHPS surveys comes from a person-centered viewpoint based on the patient’s perception of experience with the home health agency. This is accomplished through the use of core questions like does the agency effectively explain things to the patient in a way they understand, or do their personnel show a high level of professionalism or respect toward the patient. Framing questions this way lays a solid groundwork for comparing agencies.
HHCAHPS surveys can also effectively identify servicing gaps and suggest creative solutions in the delivery of home health care services. Such insights can lead to better financial outcomes for providers, since the CMS is providing incentives for higher levels of care, rather than paying the same rate for all, regardless of the patients’ perception of performance.
Why Use Cascade Strategies for Your HHCAHPS Surveys?
Cascade Strategies has over three decades of experience serving the health care industry. Our experience and expertise will help transform the information collected from your survey results into actionable insights, elevating the level of home health service and care you provide to make you stand out from the other agencies in addition to maximizing your financial gains from the CMS. Please visit our page describing our HHCAHPS Survey Services here, and let us know how we can help you. Also feel free to ask us questions using our contact form.
Copyright: Antoni Shkraba Studio
Featured and Top Image Copyrights: Andrea Piacquadio

Apr
How healthcare people can help underserved populations
jerry9789 0 comments Brand Surveys and Testing, Brandview World, Burning Questions
There’s no shortage of knowledge about the healthcare needs of underserved communities in the US such as the Hispanic, Black, American Indian/Alaska Native, and Native Hawaiian/Pacific Islander subpopulations. What may be lacking are workable and effective efforts to address these needs.
There are two main parts of this problem:
- Communication issues
- Lack of practical programs.
Communication issues
The recently-released National Healthcare Quality and Disparities Report points out that certain racial and ethnic groups that coincide with the underserved subpopulations are the most severely uninsured. See Figure 1. (Please note that the term American Indian/Alaska Native is shortened to AI/AN, and the term Native Hawaiian/Pacific Islander is shortened to NHPI.)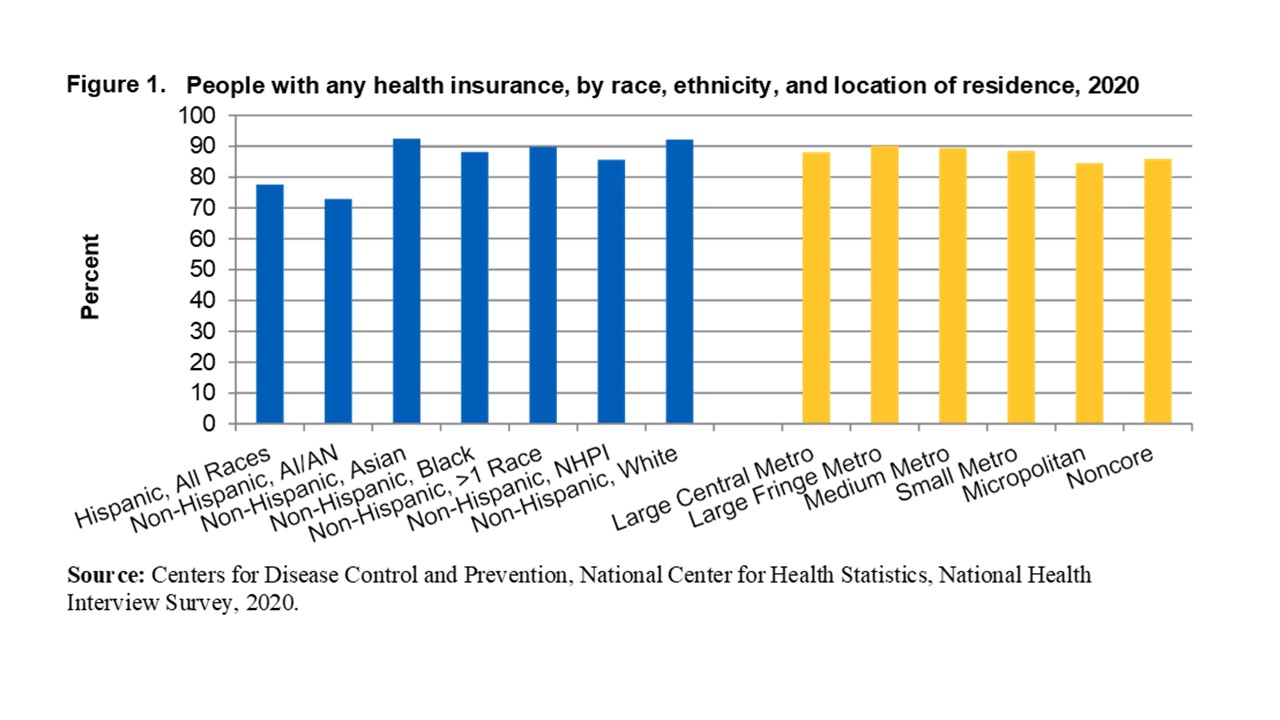 These disparities should not exist by definition, largely because of the availability of Medicare, Medicaid, and low-cost or no-cost insurance from state insurance exchanges. As the report points out, they exist largely due to communication and access issues. Many members of the underserved communities either have coverage but avoid seeking care or don’t know they’re eligible for coverage in the first place.
These disparities should not exist by definition, largely because of the availability of Medicare, Medicaid, and low-cost or no-cost insurance from state insurance exchanges. As the report points out, they exist largely due to communication and access issues. Many members of the underserved communities either have coverage but avoid seeking care or don’t know they’re eligible for coverage in the first place.
Avoiding treatment
Having coverage and avoiding care is a solvable problem, if healthcare organizations and the society in general have the will to do so. People in the underserved communities often miss planned appointments for certain medical purposes such as wellness exams, follow-up appointments, and scheduled appointments for priority services such as prenatal care and maternal wellness, causing them in the latter case to pay a high price in terms of maternal morbidity and neonatal health. (See “Lack of Practical Programs” below.) Some of this is due to language barriers, transportation issues, or unease in the interaction with healthcare personnel; but a great deal is due to a misunderstanding of the extent of their coverage, especially what remains due from the patient in the form of copayments, deductibles, etc.
Healthcare organizations can ease these problems by providing more and better-trained navigators as well as interpreters and translation services. They can build more outreach programs to the underserved to make them aware that in many cases they have little or nothing to pay for wellness services and planned care for medical purposes such as behavioral conditions, substance use treatment, chronic conditions, routine wellness care, and priority areas such as the above-mentioned prenatal care.
Not knowing about eligibility
The same potential remedy applies to lack of awareness of eligibility. Members of the underserved communities often don’t know that they’re eligible for coverage in the first place, and this leads to avoidance of treatment as well. More and better-trained health navigators supported by outreach programs can also go a long way toward alleviating this part of the problem.
Lack of practical programs
If communication with the underserved can be improved, it stands to reason that well-structured programs must be established to accommodate them. In other words, they have to have a place to go. Not enough imaginative or careful thought has been put into the development of these programs for underserved communities. Programs, personnel, and training are lacking in the areas of behavioral health, substance use treatment, dental care, prenatal/postpartum care, and more.
While the AHRQ report clearly identifies significant disparities in each of these areas for underserved communities, nowhere is the disparity more painful than in the area of prenatal care. See Figure 2.
The AHRQ data show that the level of care is well below acceptable levels for each of the four main underserved communities. This has unfortunately led to higher rates of maternal morbidity among these members of the underserved communities due to such conditions as eclampsia/preeclampsia, severe postpartum hemorrhage, venous thromboembolism, and other complications of pregnancy and childbirth.
While this is just one significant area of disparity in quality of care for the underserved, it appropriately points out the need for practical programs. Health care organizations can respond with energy and creativity by developing doula/monitrice services, transportation services, language/interpretive services, and structured prenatal and postpartum care services in tandem with the improved communication and health-navigator programs mentioned above. There’s also evidence that the provision of team-based, interprofessional, central location care centers can often lead to improved medical outcomes for underserved populations.
Information-gathering is an important first step
Clearly, different approaches will be required based on geographic, cultural, linguistic, and sociodemographic issues that pertain to your organization, but the journey always begins by gathering information. Cascade Strategies has a great deal of expertise and experience in helping healthcare companies assemble this knowledge, and we stand ready to assist you. Please tell us about your information needs at contact Cascade Strategies, and we’ll be pleased to serve your needs.